Yash Paul Chaudhry, DO1; Hunter Hayes, DO1; Efstratios Papadelis, DO1; Thomas Muzzonigro, DO1; Kenneth Wojnowski, DO2; Jackson Harvi, BS1; Andrew Star, MD3
1Philadelphia College of Osteopathic Medicine
2University of Massachusetts Chan School of Medicine
3Rothman Institute
DOI: 10.70709/PL9234-ZA
Conflicts of Interest and Disclosures
There are no commercial or funding associations for any of the authors that might pose a conflict of interest. The authors have nothing further to disclose.
Funding
Funding for this study was made possible by the Osteopathic Research and Education for Orthopedics (ORE-O) Grant from the American Osteopathic Foundation and the American Osteopathic Academy of Orthopedics Foundation.
Abstract
Background
Total knee arthroplasty (TKA) patients are frequently subjected to immediate postsurgical pain and sleep disruption. Recent studies have explored postoperative sleep disruption using subjective assessments, however the literature on objective sleep quality markers remains sparse.
Purpose
The aim of this pilot study was to assess objective sleep quality measures in the immediate postoperative period following TKA.
Design/Methods
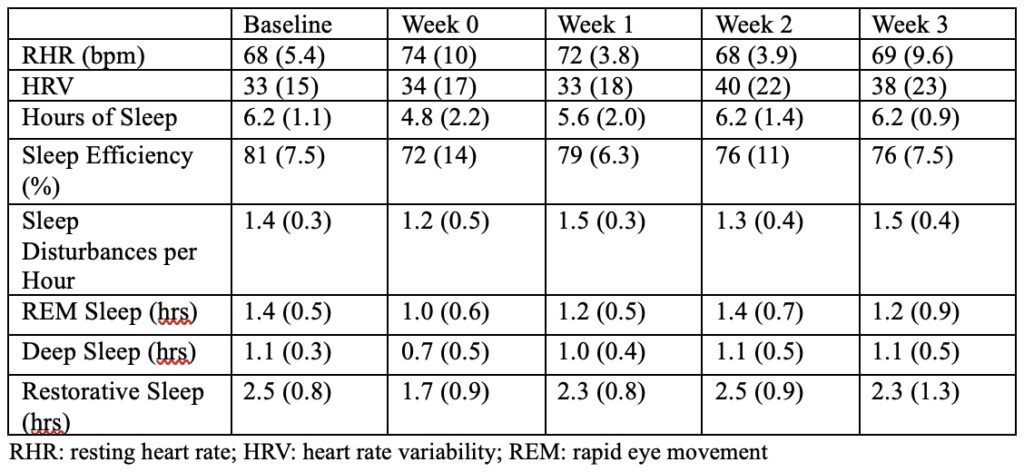
Patients undergoing primary TKA at a level two medical center were enrolled in a prospective study. Wearable sleep tracking devices (WHOOP, USA) were used to record resting heart rate (RHR), heart rate variability (HRV), hours of sleep, number of sleep disturbances per hour, hours of deep sleep (N3), hours of rapid eye movement (REM) sleep, and restorative sleep (deep and REM sleep combined) for at least a week preoperatively and four weeks postoperatively. The mean preoperative baseline values were compared to mean values over the first four postoperative weeks.
Results
Out of 25 enrolled patients, eight patients with complete data were included for analysis,. The mean hours of deep sleep (0.7 vs. 1.1; p=0.043) and restorative sleep (1.7 vs 2.3; p=0.043) were decreased in the first postoperative week compared to the fourth postoperative week. There were no other significant differences regarding any other outcomes.
Conclusion
This pilot study suggests that TKA patients have disruptions in deep and restorative sleep in the immediate postoperative period, although the sample size was limited by patient compliance with the wearable devices. Further study with greater sample size is warranted to further explore trends in postoperative sleep quality.
Keywords: total knee arthroplasty; sleep quality; wearable technology
Introduction
As the incidence of total knee arthroplasty (TKA) increases in the United States, there has been a recent emphasis on perioperative sleep quality and how it may affect patient satisfaction [1, 2]. The quality and quantity of sleep is adversely affected by a multitude of contributing factors: pain, opioid administration, anxiety, severity of surgical trauma, and environmental effects [3]. Night pain specifically has been reported in up to 50% of patients undergoing TKA, particularly in the first three nights [4]. Some of these may even play a synergistic role in disturbing sleep; opioids administered at night have been linked to respiratory disturbances such as the impairment of ventilatory response and depression of respiratory function that lead to poor sleep quality [5-7]. It has been suggested that this pain leads to a self-propelling cycle of poor sleep quality that further contributes to hyperalgesia [8]. If not managed, postoperative sleep disturbance can lead to delayed patient recovery and increased morbidity [3]. Due to these wide variety of factors such as pain, medication administration, stress and anxiety, surgical patients have an increased amount of sleep fragmentation on postoperative night 1 and 2, with a reduction in deep, slow wave sleep (N3) and REM. REM rebound may occur on postoperative day 3 to 5, leading to more severe episodes of apnea and hypoxemia, especially in patients with undiagnosed obstructive sleep apnea. While sleep disturbance is well characterized with regards to its effect on the sleep cycle, its effects on patients undergoing TKA are not as well understood. With nearly twenty percent of patients reporting dissatisfaction after TKA, sleep quality remains a poorly studied field with regards to its effect on arthroplasty [9]. Most of the existing literature focuses on subjective assessments [8, 10], which are limited as patient perception of sleep quality is poor and can be affected by several confounding factors, particularly in elderly patients who may be more likely to undergo TKA [11, 12]. The aim of this pilot study was to assess objective markers of sleep quality in the acute perioperative period and characterize how it is affected by the recovery process.
Methods
A prospective study was performed on patients undergoing primary unilateral total knee arthroplasty between May 2022 and May 2023 at a single level two tertiary care hospital by a single surgeon. Patients were recruited in clinic during preoperative visits. Subjects were informed about potential risks and benefits of the study and written consent was obtained for all participants prior to enrollment. Patients between the ages of 55-80 undergoing primary unilateral TKA for a diagnosis of osteoarthritis were eligible for inclusion in this study. Exclusion criteria included revision TKA, bilateral TKA, patients who did not own a smartphone, and a diagnosis of sleep apnea.
Patients enrolled in the study were assigned a WHOOP® brand wearable biometric tracking device that was paired with their smartphone (WHOOP, USA). This wearable wrist strap has been validated in previous studies as a reasonable method for sleep estimation, particularly when polysomnography is difficult to implement [13, 14]. WHOOP uses an accelerometer to detect movement changes and determine sleep versus wake in the form of actigraphy, and also contains LED light paired with photodiodes to obtain photoplethysmography data and estimate heart rate related variables. WHOOP’s proprietary algorithm determines sleep staging. When compared to the gold standard in polysomnography, WHOOP similarly accurately estimates sleep versus wake and overall timing of sleep but is less reliable when attempting to determine the specific sleep stage. Compared to ECG derived metrics, WHOOP accurately measures heart rate and heart rate variability [15]. The patients were instructed to wear their devices at night for at least one week preoperatively and for four weeks after surgery. Data abstracted from the device included resting heart rate (RHR), heart rate variability (HRV), hours of sleep, sleep efficiency (percentage of time spent sleeping while in bed), number of sleep disturbances per hour of sleep, hours of rapid eye movement (REM) sleep, hours of deep (slow wave) sleep, and hours of restorative sleep (deep and REM sleep). A mean value was generated for each outcome for the preoperative baseline, week 0 (postoperative days 0-6), week 1 (postoperative days 7-13), week 2 (postoperative days 14-20), and week 3 (postoperative days 21-27).
All procedures were performed under spinal anesthesia with a tourniquet through a midvastus approach with utilization of robotic assistance. Patients enrolled in the study spent one night in the hospital after surgery and were discharged on postoperative day 1. All patients were subject to a multimodal pain regimen including standing acetaminophen and ketorolac with as needed tramadol for mild pain, oxycodone for moderate pain, and intravenous hydromorphone for breakthrough pain.
All results were described as mean ± standard deviation (SD). Patients were excluded from analysis if they did not wear the device preoperatively to establish a baseline or if they did not have complete data for at least one week postoperatively. The Mann-Whitney U test for independent samples was used for unpaired comparisons of all outcomes between preoperative baseline and the first, second, and third weeks after surgery. Statistical significance was set at p < 0.05.
This study was approved by our institutional review board. Written informed consent was obtained from all subjects included in this study.
Results
A total of twenty-five patients were successfully recruited to participate in this study. Thirteen patients initially agreed to the study but did not wear their devices once recruited. An additional four patients either did not have preoperative baseline data or any postoperative data. The resulting eight patients were included for analysis in this study. The mean age of patients was 65 (10), with a mean BMI of 34 (4.2). Five of the eight patients were female.
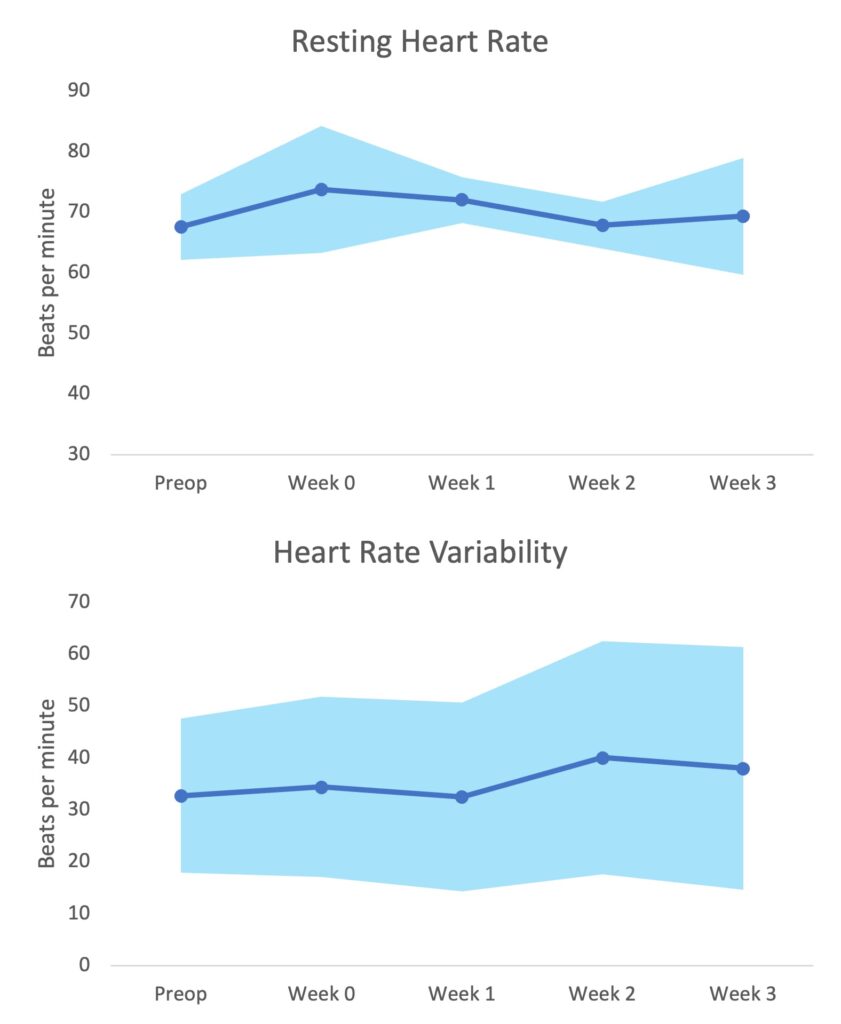
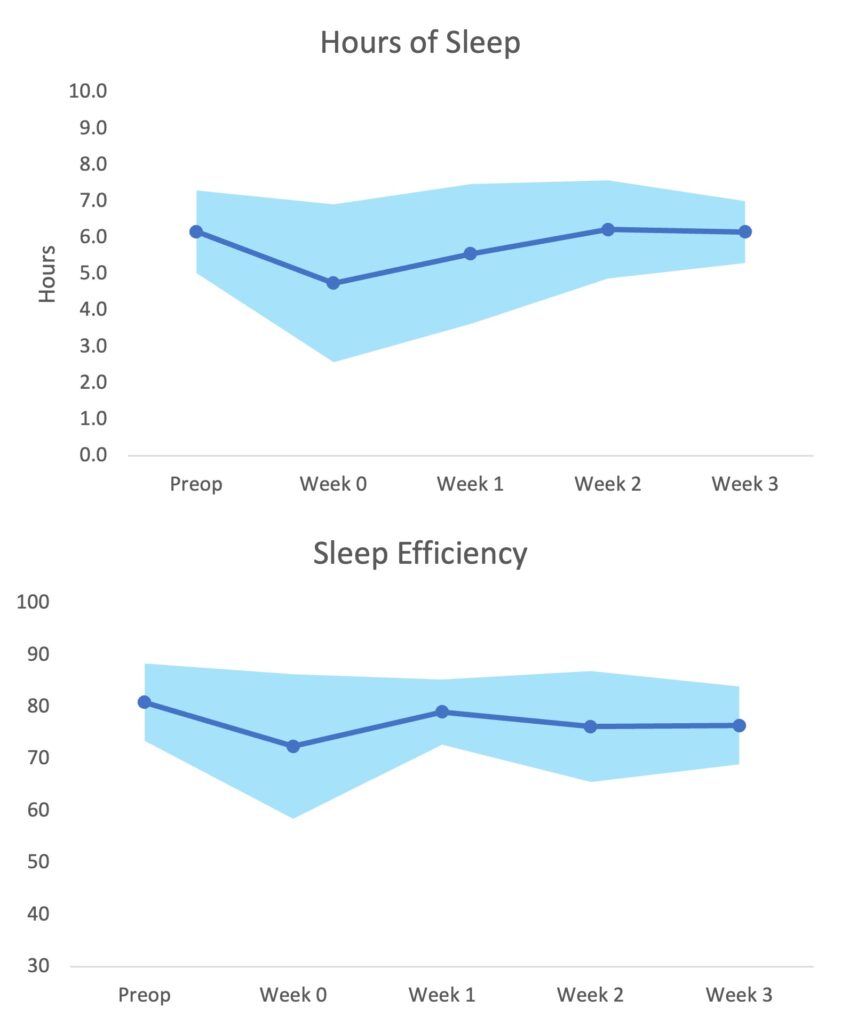
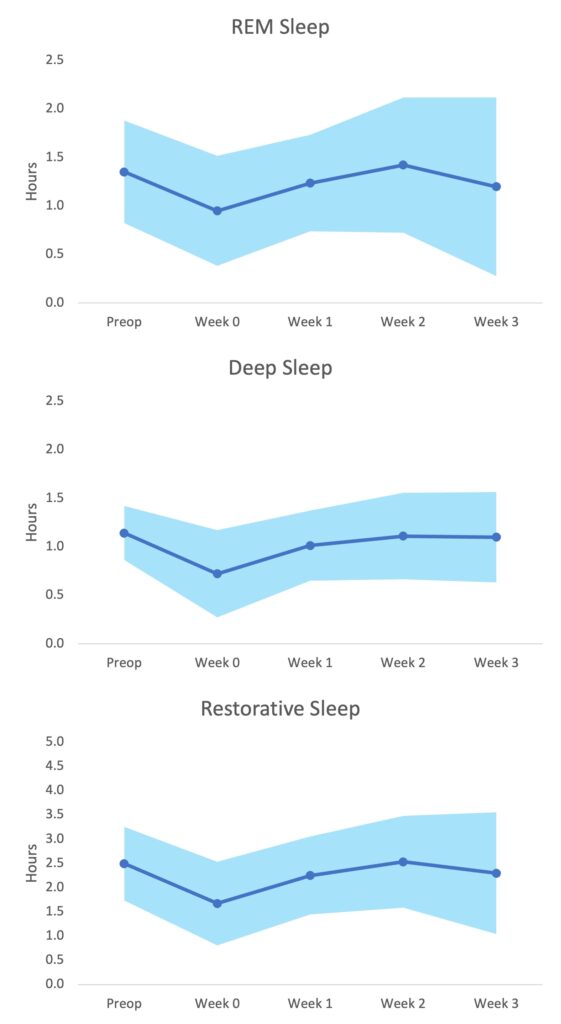
Patients averaged 6.2 hours of sleep at baseline, this decreased to 4.8 hours at week 0, then increased to 5.6 at week 1 before returning to 6.2 hours at weeks 2 and 3. However, these differences were not statistically significant. Compared to the preoperative baseline, the mean hours of deep sleep (0.7 vs. 1.1; p = 0.043) and restorative sleep (1.7 vs. 2.3; p = 0.043) were decreased in the fourth postoperative week (Table 1). There were no other differences with regards to resting heart rate, heart rate variability (Figure 1), hours of sleep, sleep efficiency (Figure 2), sleep disturbances per hour, or hours of REM sleep (Figure 3). Resting heart rate trended down from the preoperative baseline during the first two postoperative weeks, and sleep efficiency, and hours of REM sleep trended towards decreased values during the first two postoperative weeks as well, but these differences were not statistically significant.
Discussion
This pilot study demonstrates the efficacy of tracking objective measures of sleep in primary total knee arthroplasty patients in the perioperative period. Despite the low sample size in this pilot study, the hours of sleep spent in deep sleep and restorative sleep were significantly less in the first week after surgery, returning to baseline levels after the initial week. No differences were found at any time points with regards to the other variables. The limited patient compliance suggests that a more user-friendly device may be needed for any further examination of objective sleep quality markers in future studies. The role of sleep after TKA is crucial as improved sleep quality has been linked to decreased pain and use of opioid analgesics postoperatively [8]. As sleep quality is increasingly recognized as a crucial aspect of a successful outcome after TKA [16, 17], we hope the results of this study will aid in the development of further interventions to increase patient satisfaction.
An advantage of the current study is the use of objective markers of sleep. While there is abundant literature on subjective measures of sleep such as the Pittsburgh Sleep Quality Index (PSQI), self-assessment of sleep quality is notably unreliable and does not always correlate with objective measures, particularly in older patients [11]. There are a host of potential confounders such as ethnicity or pre-existing psychological factors such as catastrophizing that may affect self-reported sleep quality [18]. Additionally, by breaking hours of sleep down further into stages the current study was able to assess the amount of time spent in REM and deep sleep, which can be useful to study as it has demonstrated links to subjective sleep quality, cognitive ability, and pain perception [19, 20]. While there are few studies examining objective sleep measures in TKA patients, their findings appear to line up with those of the current study [4, 21]. One study performed by Krenk et. al. in Denmark in 2012 involving ten patients undergoing TKA or total hip arthroplasty (THA) used polysomnography to assess sleep architecture [21]. They established a baseline one night before surgery at the patient’s home, during the hospitalization, and on the fourth postoperative night again at the patient’s home. Similar to our study, they found that the proportion of REM sleep per night was significantly less immediately after surgery but normalized on the fourth postoperative night. However, their study included both THA and TKA patients, which is of particular concern as TKA patients have been demonstrated to have significantly greater pain levels and sleep disturbance postoperatively [4]. Additionally, due to the limitations involved in setting up polysomnographic testing, the baseline and postoperative home visits in their study were based on single night studies as opposed to testing over several nights’ worth of sleep. Another study performed by Gibian et. al. in 2023 used FitBitÆ devices to track hours of sleep and sleep disturbances for 12 weeks postoperatively [22]. While they were unable to examine different stages of sleep, they did not find any differences in total hours of sleep between baseline and at their 30, 60, and 90-day points postoperatively. Of note, they did report worsened subjective PSQI scores at 30 days but improved beyond baseline at 90 days.
Subjective sleep measures have been extensively studied in arthroplasty literature; however they are less commonly used in the acute perioperative period. Meirhaeghe et. al. collected a short form of the PSQI (one question on sleep duration, one on sleep quality) in 780 THA and TKA patients at one year and found that 74% of patients reporting poor sleep quality preoperatively noted significant improvements at one year [2]. Satisfaction was much higher in patients reporting good quality sleep as opposed to those reporting bad sleep quality (93% vs 78%). In a prospective study of 34 TKA patients, Chen et. al. reported a decrease in PSQI scores from baseline to the postoperative 6-week mark [1]. However, they also found that this decrease in sleep quality was transient and reversed at 3 months, with scores significantly improved from baseline at this point. Koken et. al. reported differing results in a retrospective study of 80 TKA patients who underwent PSQI testing, finding no difference between sleep quality when comparing preoperative baseline and postoperative 6-week values [23]. They did find an increase in sleep quality at six months, however. These differing results with regards to subjective measures may be attributed to the multifactorial nature of perceived sleep. Additionally, the most commonly used survey in sleep literature, the PSQI, is designed in a way to have the subject consider their sleep quality over the past month [12]. This makes it less ideal as a tool to capture perioperative sleep quality, which according to the results of the current study may be dramatically different in the first postoperative week than two or three weeks after surgery.
Limitations
The most prominent issue with the current study was the sample size. Asking patients to wear a device to sleep every night for multiple weeks was often perceived as a burdensome request. Patients who did not wear the devices may have done so either due to forgetting about them or because they found the devices bothersome. In recognition of the burden of wearing this device every night, we chose a four-week period to assess sleep markers as opposed to anything longer. While it appears that sleep quality returns to baseline as assessed by objective markers by four weeks, further study may be warranted to assess how it changes over a longer period of time. In addition, it required patients to understand how to charge the device and pair it with their smartphone. As a result, the current study often had poor compliance that limited the number of patients with complete data. Additionally, despite follow-up calls to assist in increasing patient compliance, several patients had to be excluded from analysis due to missing data either preoperatively or postoperatively. This may indicate that the objective measurement of sleep after TKA may require a more user-friendly device or one that requires minimal patient involvement. While several variables appeared to show a difference between baseline and immediate postoperative values such as RHR, HRV, sleep score, and hours of sleep, the low sample size may have limited the ability to expose any statistical differences between these values. Further limitations include the lower accuracy of sleep wearables to determine specific sleep staging when compared to the gold standard polysomnography. Also, the mean BMI of our patients was 34, which puts them at higher risk for having underlying undiagnosed obstructive sleep apnea and sleep disturbance at baseline. One of the strengths of the study is that the non-intrusive nature of the device allows for its use every day of the perioperative period, as compared to polysomnography which requires a much more extensive set up.
Conclusion
The results of this study suggest that patients undergoing TKA have disruptions in deep and restorative sleep in the immediate postoperative period. These findings can be used to help providers discuss expectations for the postoperative experience after TKA with their patients. Additional studies with larger sample sizes are warranted to further delineate the course of sleep quality after surgery, the factors related with poor sleep quality, and the efficacy of medical or cognitive interventions that may assist in improving it.
Acknowledgements and Disclosures
Author Contributions
- YP: conceptualization; formal analysis; funding acquisition; investigation; methodology; project administration; writing – original draft, writing – review and editing
- HH: conceptualization; methodology; writing – original draft; writing – review and editing
- EP: conceptualization; methodology; writing – original draft; writing – review and editing
- TM: writing – original draft; writing – review and editing
- KW: writing – original draft; writing – review and editing
- JH: conceptualization; investigation; methodology; data curation
- JH: formal analysis; methodology; visualization; writing – original draft
- AS: conceptualization; methodology; supervision; writing – review and editing
Funding Sources
Funding for this study was made possible by the Osteopathic Research and Education for Orthopedics (ORE-O) Grant from the American Osteopathic Foundation and the American Osteopathic Academy of Orthopedics Foundation.
References
- Chen AF, Orozco FR, Austin LS, Post ZD, Deirmengian CA, Ong AC. Prospective Evaluation of Sleep Disturbances After Total Knee Arthroplasty. J Arthroplasty 31(1): 330, 2016
- Van Meirhaeghe JP, Salmon LJ, O’Sullivan MD, Gooden BR, Lyons MC, Pinczewski LA, Roe JP. Improvement in Sleep Patterns After Hip and Knee Arthroplasty: A Prospective Study in 780 Patients. J Arthroplasty 36(2): 442, 2021
- Rampes S, Ma K, Divecha YA, Alam A, Ma D. Postoperative sleep disorders and their potential impacts on surgical outcomes. J Biomed Res 34(4): 271, 2019
- Wylde V, Rooker J, Halliday L, Blom A. Acute postoperative pain at rest after hip and knee arthroplasty: severity, sensory qualities and impact on sleep. Orthop Traumatol Surg Res 97(2): 139, 2011
- Vasu TS, Grewal R, Doghramji K. Obstructive sleep apnea syndrome and perioperative complications: a systematic review of the literature. J Clin Sleep Med 8(2): 199, 2012
- Onen SH, Onen F, Courpron P, Dubray C. How pain and analgesics disturb sleep. Clin J Pain 21(5): 422, 2005
- Wang D, Teichtahl H. Opioids, sleep architecture and sleep-disordered breathing. Sleep Med Rev 11(1): 35, 2007
- Shen SP, Wang YJ, Zhang Q, Qiang H, Weng XS. Improved Perioperative Sleep Quality or Quantity Reduces Pain after Total Hip or Knee Arthroplasty: A Systematic Review and Meta-Analysis. Orthop Surg 13(4): 1389, 2021
- Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 468(1): 57, 2010
- Alipourian A, Farhadian N, Zereshki E, Khazaie H. Improvement of sleep quality 6 months after total knee arthroplasty: a systematic review and meta-analysis. J Orthop Surg Res 16(1): 342, 2021
- O’Donnell D, Silva EJ, Münch M, Ronda JM, Wang W, Duffy JF. Comparison of subjective and objective assessments of sleep in healthy older subjects without sleep complaints. J Sleep Res 18(2): 254, 2009
- Fabbri M, Beracci A, Martoni M, Meneo D, Tonetti L, Natale V. Measuring Subjective Sleep Quality: A Review. Int J Environ Res Public Health 18(3), 2021
- Berryhill S, Morton CJ, Dean A, Berryhill A, Provencio-Dean N, Patel SI, Estep L, Combs D, Mashaqi S, Gerald LB. Effect of wearables on sleep in healthy individuals: a randomized crossover trial and validation study. Journal of Clinical Sleep Medicine 16(5): 775, 2020
- Miller DJ, Lastella M, Scanlan AT, Bellenger C, Halson SL, Roach GD, Sargent C. A validation study of the WHOOP strap against polysomnography to assess sleep. Journal of Sports Sciences 38(22): 2631, 2020
- Miller DJ, Sargent C, Roach GD. A Validation of Six Wearable Devices for Estimating Sleep, Heart Rate and Heart Rate Variability in Healthy Adults. Sensors (Basel) 22(16), 2022
- Bartosiak K, Schwabe M, Lucey B, Lawrie C, Barrack R. Sleep Disturbances and Disorders in Patients with Knee Osteoarthritis and Total Knee Arthroplasty. J Bone Joint Surg Am 104(21): 1946, 2022
- Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28(2): 193, 1989
- Goodin BR, Fillingim RB, Machala S, McGuire L, Buenaver LF, Campbell CM, Smith MT. Subjective sleep quality and ethnicity are interactively related to standard and situation-specific measures of pain catastrophizing. Pain Med 12(6): 913, 2011
- Della Monica C, Johnsen S, Atzori G, Groeger JA, Dijk DJ. Rapid Eye Movement Sleep, Sleep Continuity and Slow Wave Sleep as Predictors of Cognition, Mood, and Subjective Sleep Quality in Healthy Men and Women, Aged 20-84 Years. Front Psychiatry 9: 255, 2018
- Stroemel-Scheder C, Kundermann B, Lautenbacher S. The effects of recovery sleep on pain perception: A systematic review. Neurosci Biobehav Rev 113: 408, 2020
- Krenk L, Jennum P, Kehlet H. Sleep disturbances after fast-track hip and knee arthroplasty. Br J Anaesth 109(5): 769, 2012
- Gibian JT, Bartosiak KA, Lucey BP, Riegler V, King J, Barrack RL. Sleep Disturbances Following Total Knee Arthroplasty. J Arthroplasty 38(6s): S120, 2023
- Koken M, Guclu B. The Effects of Total Knee Arthroplasty on Sleep Quality. Malays Orthop J 13(2): 11, 2019