John Michael Pirtle, DO; Chloe Myers, DO; Peyton Carlson, PA-C; Sean Conrad, PA-C; Valerie Ranone, PA-C; Amy Mills, RN; and Bryan P. Hooks, DO*
University of Pittsburgh Jameson
*Dr. Bryan Hooks is Chairman of Department of Surgery UPMC Horizon and UPMC Jameson and Fellowship Trained in Adult Reconstruction from Cleveland Clinic Foundation, Cleveland, Ohio.
DOI: 10.70709/XR567-0123
Abstract
This case report describes a case of minocycline induced black bone disease encountered during an elective total knee arthroplasty. Prior to the procedure, no history gleaned from the patient suggested concern for any osseous pathology aside from arthritic changes. In the operative suite, the articular cartilage and subchondral bone were noted to be hyperpigmented. Samples were taken for histopathology to rule out alkaptonuria as an alternative cause of this diffuse hyperpigmentation. In the post operative suite, the patient was able to confirm long standing use of high doses of minocycline for dermatologic purposes. No other pathological processes were noted from the operative samples taken. This case highlights the importance of thorough medical history, understanding of biochemical principles and broad-based differentials when unsuspecting findings are noted during routine cases. Exposure to, and reporting these types of cases are vital to future surgeon recognition of this disease process.
Keywords: Black Bone Disease, Minocycline Induced Black Bone Diseae
Introduction
Black bone disease has several causes, but two of the most common are alkaptonuria, an autosomal recessive disorder, and the use of minocycline antibiotic.4,9 Alkaptonuria is a disease whereby homogentisic acid oxidate is insufficient, causing an elevated level of homogentisic acid (HGA).4 HGA then combines with connective tissue, causing a black-pigmented appearance. A more direct cause of actual black bone is seen with long-term use of minocycline or other tetracycline antibiotics.9 These drugs can cause grey, greyish-black, brown, blue-green or black pigment changes to skin, soft tissues, cartilage or bone with chronic use. Minocycline and other tetracycline antibiotics bind with calcium, an ion that is prominent in bone and in teeth. Long term use of these antibiotics can lead to the black or blue pigment seen in bone.9 This discoloration would unlikely be encountered unless found in surgery.9 Studies have presented individuals with alkaptonuria4, minocycline induced black bone disease of the large joints2,7, temporal bones in the skull, and in the feet.6 It is important for the surgeon performing the operations to identify this abnormality and to consider evaluation for other possible causes of black stained tissues, including infection or metal ion toxicity.9
Our case focuses on the black bone disease from Minocycline. Minocycline is used as a broad-spectrum antibiotic in the tetracycline class. Specifically, the antibiotic works to inhibit the 30s subunit of the bacterial ribosome thus preventing the formation of new proteins necessary for bacterial cellular development and growth.8 Minocycline binds strongly to plasma proteins and is lipid soluble, allowing it to penetrate tissues and body fluid, resulting in a permanent discoloration.9 Off-label Minocycline uses include rosacea, acne, bullous dermatoses, and autoimmune diseases (N and Gar). Minocycline is commonly prescribed for acne, which can cause hyperpigmentation of the skin, nails, bones, thyroid, teeth, palate, eyes, and heart valves.10 Minocycline’s use in autoimmune diseases, such as rheumatoid arthritis, is supported given the antibiotics ability to reduce inflammation, but this is considered off-label use. (GAR)
Presentation of case
The case described here details a 65-year-old male patient with past medical history of essential hypertension, gastroesophageal reflux disease, deep vein thrombosis, and rosacea, who presented with classic arthritic changes to the left knee with failure of conservative management including, physical therapy, corticosteroid and viscosupplementation injections, to alleviate pain (Appendix 1-2). Our patient was consented and elected to proceed with total knee arthroplasty, and the patient was medically cleared without any contraindications to proceed with surgery.
Preoperative AP and Lateral Knee Radiographs of Our Patient Demonstrating Findings Consistent with Classic Osteoarthritis of the Left Knee, which met Criteria for Total Knee Arthroplasty
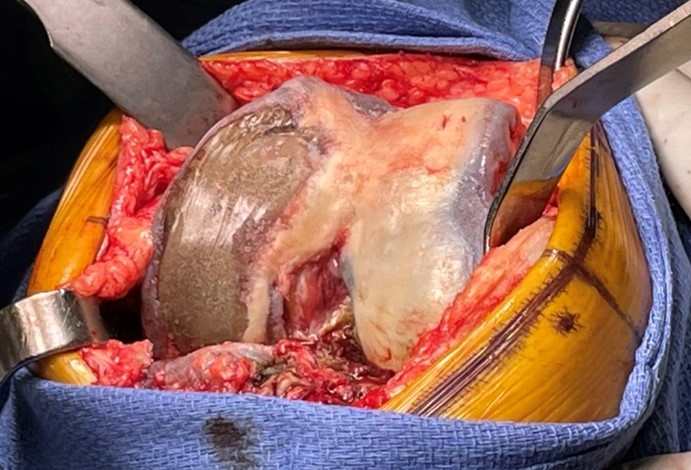
During the procedure, the articular cartilage and subchondral bone were found to be hyperpigmented (Appendix 3-4). Samples were sent for histopathology to rule out other possible causes of hyperpigmentation, including the original working diagnosis of alkaptonuria. The case proceeded without incident.

In the postoperative unit, the patient was asked about symptoms consistent with alkaptonuria including darkening of urine, kidney stones or other related kidney conditions. The patient denied these and displayed his darkened nail beds and admitted to long term usage of minocycline for rosacea. (Appendix 5).
Final pathology was found to be consistent with mild chronic synovitis with focal hemosiderin deposition. The specimen was negative for acute inflammation. An additional diagnosis of degenerative joint disease was documented. All intraoperative cultures were negative for bacterial growth. Postoperative Radiographs are seen in Appendices 6 and 7 below.



Discussion
Black bone disease has several causes, but two of the most common are alkaptonuria, an autosomal recessive disorder, and the long-term use of minocycline as seen in our patient. Minocycline can cause pigment changes to the skin and other soft tissues with chronic use, but research has shown that there can be deposition into bone. Tetracycline antibiotics bind with calcium, an ion that is prominent in bone and in teeth. Therefore, long term use of these antibiotics can lead to the black or blue pigment seen in bone.8 This discoloration is most often encountered intraoperatively. It is important for the surgeon performing the operation to identify this abnormality and be committed to rule out other possible causes of black or discolored tissues such as alkaptonuria, infection or metal ion toxicity. In the case presented here, all other possible causes of black/discolored bone were investigated and appropriately ruled out by the operative surgeon.1
On imaging, black bone disease is not seen radiographically, and is not diagnosed until surgery, when gross visualization of the joint demonstrates dark pigmentation of subchondral and cancellous bone.5 Pigmentation due to long-term use of minocycline occurs with cumulative doses of >100 gm. If hyperpigmentation occurs secondary to minocycline, the medication should be stopped to prevent further accumulation, which may or may not resolve.10 Minocycline induced disease is confirmed with histology that reveals normal bone structure despite discoloration.9 Pathology and Histology results for this patient identified normal underlying bone, which confirmed minocycline-induced black bone disease.
The other concerning diagnosis that was suspected early in this case was alkaptonuria. Alkaptonuria is a disease in which homogentisic acid oxidase is insufficient, thus causing an elevated level of homogentisic acid (HGA). HGA is then oxidized to benzoquinone acetic acid, which is later oxidized to form a melanin-like pigment that can darken connective tissues, sclera, nails, skin, bone, and cardiovascular tissues5. Over time the deleterious effects of elevated levels of HGA can cause tissue degradation with accompanying inflammatory changes5. HGA, and homogentisic acid oxidase were normal in this patient and thus ruled out alkaptonuria as a possible cause of the pigmentation.
There is no specific definitive treatment for black bone disease and few treatments other than analgesics and joint replacement are available to patients with alkaptonuria.10 In Europe, Nitisinone, a 4-hyroxyphenylpyruvate dioxygenase inhibitor, which converts HGA to pyruvic acid and slows disease progression, has been approved for use.5 Just as general arthritis, the treatment of ochronotic arthritis involves symptomatic treatment and total joint replacement. In addition, those with black bone disease may benefit from a low protein diet and the addition of vitamin C.11 By reducing protein in the diet, one will have lower levels of tyrosine and phenylalanine, resulting in less HGA production. Vitamin C aids in reducing oxidation of benzoquinone acetic acid and the formation of free radicals.5
McCleskey et al7, described a case of an 81-year male with a 5-year history of severe, progressive pain in the right knee with a past medical history significant for rosacea, whereby he took minocycline 50mg twice a day over a two-year period. After failed nonoperative treatment, he met criteria for total knee arthroplasty. He was followed by dermatology, who diagnosed him with minocycline-induced hyperpigmentation and was advised to stop taking the medication one month before surgery. Specimens were collected and sent to pathology during his total knee arthroplasty, which revealed osteoarthritis, and embedded patches of fluorescence, consistent with minocycline deposition over time. Total knee arthroplasty was performed as planned and fixated with cement. At his one year follow up, the patient had excellent joint stability, components were secure and aligned, and he was doing well.7
A case report by Vermeijden et al12, discuss a 19-year-old male with history of acne treated for three years with 105mg minocycline daily who underwent a revision anterior cruciate ligament and medial meniscal repair. During surgery there was extensive dark brown synovitis, and severe brown-black hyperpigmentation of the cortical bone so debridement and synovectomy with biopsy was sent for cultures. Histopathological analysis resulted in abundant pigment laden macrophages in the cortical bone and synovial lining, which stained positive with iron stain, indicating the pigment as minocycline-related type 2 pigmentation. A month later, the ACL reconstruction was completed without complications. At follow up six years later, the patient still had a stable Lachman exam, full range of motion and was doing well.12
Kerbleski et al6 describes a case report in which a 49-year-old male with a 15-year history of minocycline use for acne underwent hallux rigidus corrective surgery after failing nonoperative treatment. Preoperative radiographs demonstrated severe first metatarsophalangeal joint osteoarthritis. Intraoperatively, dark discoloration of the osseous tissue and central cartilage of the first metatarsal and proximal phalanx was encountered. Pathology of the bone specimens revealed grossly discolored bone and no signs of inflammation or necrosis. He was diagnosed with long-term minocycline induced hyperpigmentation of bone. He had a normal and expected postoperative period and recovery at 6-months postoperatively.6
Conclusion
Our patient was found to harbor black bone disease secondary to long-term usage of the antibiotic minocycline. While the etiology was unknown intraoperatively, precautions were taken to guide diagnosis and rule out infection. The patient has since followed up and has done well with his knee replacement. Due to the nature of this case, the authors recognize the importance of full medication review to identify potential causes of hyperpigmentation, to help streamline intraoperative decision making. These side effects must also be appropriately discussed with patients by the prescribing physician, so patients can understand inherent risk. Our patient successfully underwent total knee arthroplasty for osteoarthritic symptoms, with the incidental finding of minocycline induced hyperpigmentation, and he fortunately has had no systemic or adverse sequelae with his pain-free knee.
Minocycline Case Report References
- Antonenko YN, Rokitskaya TI, Cooper AJL, Krasnikov BF. Minocycline chelates Ca2+, binds to membranes, and depolarizes mitochondria by formation of Ca2+-dependent ion channels. J Bioenerg Biomembr. 2010;42(2):151-163. doi:10.1007/s10863-010-9271-1
- Ashukem M, Levy J, Formaini N. Minocycline induced black bone disease: An incidental finding during total shoulder arthroplasty. Curr Orthop Pract. 2016;27:698-701. doi:10.1097/BCO.0000000000000439
- Garrido-Mesa N, Zarzuelo A, Gálvez J. Minocycline: far beyond an antibiotic. Br J Pharmacol. 2013;169(2):337-352. doi:10.1111/bph.12139
- Harun M, Hayrettin Y, Serhat M, Cuneyt M, Fırat F, Ufuk O. A rare cause of arthropathy: An ochronotic patient with black joints. Int J Surg Case Rep. 2014;5(8):554-557. doi:10.1016/j.ijscr.2014.06.015
- Kang HW, Kim M, Oh JY, Youn C. Black Bone Disease: Ochronotic Arthritis Detected during Knee Arthroplasty. J Bone Metab. 2023;30(3):283. doi:10.11005/jbm.2023.30.3.283
- Kerbleski GJ, Hampton TT, Cornejo A. Black bone disease of the foot: a case study and review of literature demonstrating a correlation of long-term minocycline therapy and bone hyperpigmentation. J Foot Ankle Surg Off Publ Am Coll Foot Ankle Surg. 2013;52(2):239-241. doi:10.1053/j.jfas.2012.10.018
- McCleskey PE, Littleton KH. Minocycline-induced blue-green discoloration of bone. A case report. J Bone Joint Surg Am. 2004 Jan;86(1):146-8. doi: 10.2106/00004623-200401000-00023. PMID: 14711958.
- Nazarian S, Akhondi H. Minocycline. In: StatPearls. StatPearls Publishing; 2024. http://www.ncbi.nlm.nih.gov/books/NBK554519/
- Steadman W, Brown Z, Wall CJ. Minocycline black bone disease in arthroplasty: a systematic review. J Orthop Surg. 2021;16(1):479. doi:10.1186/s13018-021-02617-w
- Suwannarat P, Phornphutkul C, Bernardini I, Turner M, Gahl WA. Minocycline-induced hyperpigmentation masquerading as alkaptonuria in individuals with joint pain. Arthritis Rheum. 2004;50(11):3698-3701. doi:10.1002/art.20606
- Thiam D, Teo TY, Malhotra R, Tan KB, Chee YH. Black bone disease in a healing fracture. BMJ Case Rep. 2016;2016:bcr2015211915. doi:10.1136/bcr-2015-211915
- Vermeijden HD, van der List JP, Chen YT, DiFelice GS. Minocycline-induced black bone disease with synovial pigmentation in a patient undergoing revision anterior cruciate ligament surgery: A case report. Int J Surg Case Rep. 2021;81:105819. doi:10.1016/j.ijscr.2021.105819